Table of Contents
Healthcare has always revolved around the doctor-patient relationship. Traditional care relies on in-person visits, physical records, and follow-up phone calls.
While this approach has served patients for decades, it comes with limits such as delayed diagnosis, higher costs, and accessibility issues for rural populations. AI-powered solutions are at the rescue.
Remote Patient Monitoring (RPM) software is changing that equation. By combining wearable devices, mobile apps, and cloud-based platforms, RPM brings healthcare into patients’ homes.
Doctors can track vitals in real-time, and patients receive care without frequent hospital visits. This blog compares RPM software with traditional methods, highlighting differences, advantages, and what the future holds.
What is Remote Patient Monitoring Software?
Remote Patient Monitoring (RPM) software connects patients and doctors through digital technology. It uses smart devices and applications to track vital signs such as:
- Heart rate
- Blood pressure
- Oxygen levels
- Glucose readings
- Sleep patterns
Data is sent securely to healthcare providers who can analyze trends, send alerts, or suggest treatment changes. For patients with chronic illnesses like diabetes, heart disease, or hypertension, RPM reduces the need for constant in-person visits.
Key components include:
- Wearable devices like fitness trackers or medical-grade sensors.
- Mobile apps that collect and transmit data.
- Healthcare dashboards where doctors monitor patient progress.
- AI and analytics that identify risks before emergencies occur.
RPM software makes healthcare proactive instead of reactive, allowing timely intervention.
Explore our Healthcare Software Development Solutions!
What are Traditional Care Methods?

Traditional care focuses on physical presence and manual processes. It includes:
- Regular visits to clinics or hospitals.
- Doctor assessments are based on symptoms reported during appointments.
- Paper-based or electronic medical records are updated after each visit.
- Limited communication outside appointments, usually through phone calls.
While this method builds strong human connections, it has challenges:
- Patients often wait weeks for appointments.
- Chronic condition monitoring requires repeated visits.
- Emergency response may be delayed without prior data.
- Doctors rely on self-reported information, which may lack accuracy.
Traditional care remains vital but struggles to meet the growing demand for real-time, continuous healthcare support.
Key Differences Between RPM and Traditional Care
Here’s a detailed comparison:
| Aspect | Remote Patient Monitoring (RPM) | Traditional Care Methods |
| Accessibility | Patients receive care at home through connected devices | Requires physical visits to hospitals/clinics |
| Data Availability | Continuous, real-time tracking of vitals | Data recorded only during appointments |
| Cost Efficiency | Fewer hospital visits reduce costs | Frequent in-person visits increase expenses |
| Response Time | Alerts allow quick interventions | Emergency response depends on appointment timing |
| Patient Engagement | Interactive apps and devices keep patients active | Engagement mainly during visits |
| Chronic Disease Care | Effective for long-term monitoring | Requires regular clinic trips |
| Record Keeping | Cloud-based, accurate, and centralized | Manual, fragmented across providers |
Explanation:
RPM provides better accessibility, lowers costs, and supports preventive care. Traditional methods, while personal, lack continuous data and often delay treatment adjustments.
Technologies Used in Remote Patient Monitoring (RPM)
Remote Patient Monitoring combines different technologies to connect patients and doctors. Each plays a role in collecting, transmitting, and analyzing health data.
1. Wearable Devices
- Smartwatches, ECG patches, and glucose monitors track vitals such as heart rate, oxygen levels, and blood sugar.
- Devices are designed to be non-intrusive and patient-friendly.
2. Mobile Applications
- Apps connect wearable devices to healthcare systems.
- They display readings to patients and send real-time data to providers.
- Patients can also log symptoms or medication intake directly.
3. Cloud Platforms
- Centralized platforms store patient data securely.
- Doctors access dashboards to analyze patterns and make treatment decisions.
- Scalable cloud systems allow multiple patients to be monitored simultaneously.
4. IoT Connectivity
- Internet of Things (IoT) technology links devices and apps.
- Bluetooth, Wi-Fi, and cellular networks enable smooth data transfer.
- Continuous connectivity makes RPM reliable across locations.
5. Artificial Intelligence and Analytics
- AI algorithms detect anomalies in patient data.
- Predictive analytics help identify risks before emergencies occur.
- Machine learning models refine treatment recommendations over time.
6. Integration with Electronic Health Records (EHR)
- RPM platforms connect with hospital EHR systems.
- This integration ensures doctors have a complete patient history when making decisions.
Advantages of Remote Patient Monitoring Over Traditional Care
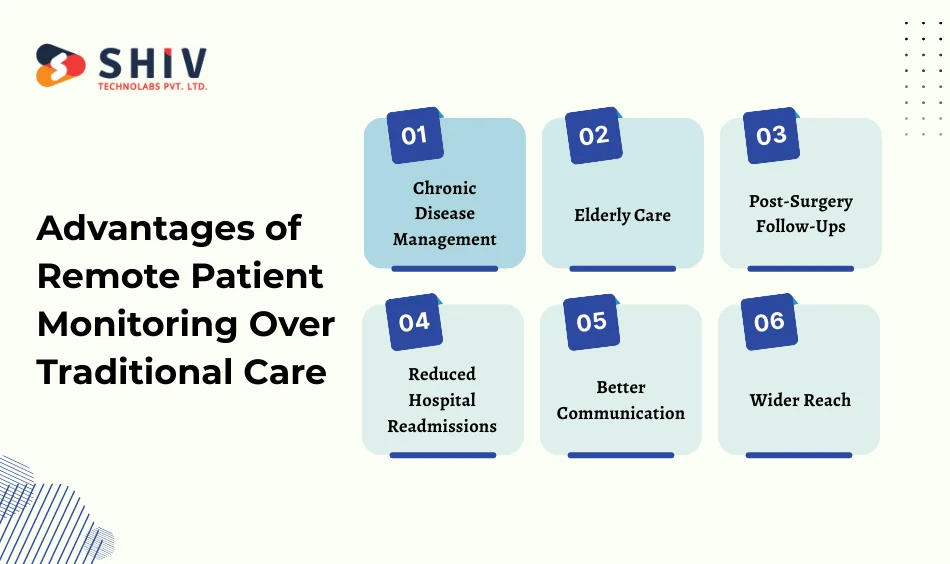
- Chronic Disease Management: Patients with diabetes, hypertension, or heart disease need regular tracking. RPM reduces hospital visits and keeps treatment plans updated.
- Elderly Care: Older patients often struggle with mobility. RPM allows them to stay at home while doctors monitor their health remotely.
- Post-Surgery Follow-Ups: Instead of multiple hospital trips after surgery, patients can share progress through connected devices. Any unusual sign can trigger a doctor’s intervention.
- Reduced Hospital Readmissions: Hospitals face penalties for high readmission rates. With RPM, early warnings help avoid complications that might lead to rehospitalization.
- Better Communication: Patients feel reassured knowing their data is constantly monitored. This builds trust and encourages treatment adherence.
- Wider Reach: RPM brings healthcare to rural or underserved regions where hospitals are scarce. Patients receive the same level of care as urban populations.
Challenges of Remote Patient Monitoring
Despite its benefits, RPM is not free from challenges:
- Data Privacy Concerns: Patients worry about sensitive medical data being exposed. Strong encryption and compliance with healthcare regulations are necessary.
- Technical Literacy: Not all patients are comfortable using digital devices. Training and user-friendly design are essential.
- Device Costs: Wearables and connected devices can be expensive, making adoption difficult for some.
- Internet Connectivity: RPM depends on reliable internet, which may not be available in remote areas.
These challenges highlight why RPM works best as a supplement to traditional care, not a replacement.
Case Studies & Real-World Applications
- Heart Disease Monitoring: Hospitals use connected ECG devices that transmit data to cardiologists. Early detection of irregularities reduces the risk of heart failure.
- Diabetes Management: Continuous glucose monitors send sugar level data directly to doctors. Patients receive diet and medicine adjustments without in-person visits.
- COVID-19 Monitoring: During the pandemic, RPM helped track oxygen levels and heart rates of patients recovering at home. This reduced hospital overcrowding.
- Remote Clinics in Rural Areas: In countries with limited healthcare access, RPM devices connect patients with urban doctors, bridging the care gap.
These examples show RPM’s practical role in improving outcomes while reducing healthcare system burdens.
Future of Healthcare with RPM
The future points to hybrid care—traditional methods supported by RPM. Some trends include:
- AI-Powered Analytics: AI can predict patient risks before symptoms appear, giving doctors more control.
- Telemedicine Integration: Video consultations combined with RPM provide complete remote care experiences.
- Predictive Healthcare: By analyzing trends, doctors can prevent diseases instead of only treating them.
- Connected Ecosystems: Hospitals, pharmacies, and insurance providers will share RPM data for coordinated healthcare.
Shiv Technolabs – Your Partner in Healthcare Software Development
At Shiv Technolabs, we design custom healthcare software that brings patient care closer to home. Our team develops Remote Patient Monitoring solutions that integrate devices, mobile apps, and cloud systems for real-time health tracking.
We focus on:
- HIPAA-compliant and secure platforms.
- Easy-to-use patient and doctor dashboards.
- Integration with existing healthcare systems.
- Custom features tailored for hospitals, clinics, and startups.
Whether you need a full-featured RPM platform or specific modules, Shiv Technolabs can deliver solutions that improve care delivery while maintaining data security.
Conclusion
Remote Patient Monitoring software is not about replacing doctors or traditional care—it’s about complementing it.
While traditional care builds strong personal bonds, RPM provides data-driven, continuous support. Together, they create a healthcare system that is faster, more accurate, and more accessible.
Healthcare providers considering RPM software can achieve better patient outcomes and lower operational costs. The shift is already underway, and those who adopt hybrid models will lead the future of patient care.
FAQs
1. What is the main difference between RPM and traditional care?
RPM tracks patient vitals in real-time through devices and apps, while traditional care relies on scheduled visits and in-person consultations.
2. What is the RPM program in healthcare?
An RPM program is a structured system where hospitals or clinics provide patients with devices and apps to track vital signs.
The collected data is securely transmitted to healthcare providers, who review it and adjust treatment plans as needed. These programs are often used for chronic illnesses like diabetes, hypertension, or heart disease.
3. How accurate is remote patient monitoring?
The accuracy of RPM depends on the quality of devices and correct usage by patients. Medical-grade wearables and sensors are highly reliable and approved by regulatory bodies.
While minor variations may occur, RPM provides far more continuous and practical data than occasional in-clinic checks.
4. Can RPM completely replace traditional care?
No. RPM is best used as a supplement. Some treatments and diagnoses still require physical visits and direct doctor interaction.
5. What features should a good RPM software have?
Key features include wearable device integration, cloud-based dashboards, secure data transfer, AI analytics, and patient-friendly mobile apps.
6. Does RPM software comply with healthcare regulations?
Yes, when developed with HIPAA or GDPR compliance standards, RPM platforms keep patient data secure.
7. What conditions benefit most from RPM?
Chronic illnesses like diabetes, hypertension, heart disease, and post-surgery recovery cases benefit most from RPM solutions.
8. Is RPM affordable for small clinics?
Many vendors offer modular solutions, allowing small clinics to adopt RPM without heavy investments.